Navigating United Healthcare Claim Submission: A Comprehensive Guide
Submitting claims to United Healthcare can often feel like navigating a complex maze. Whether you’re a healthcare provider or a patient seeking reimbursement, understanding the intricacies of the United Healthcare claim submission process is crucial for timely and accurate processing. This comprehensive guide will break down the steps involved, common pitfalls to avoid, and essential tips to ensure your claims are handled efficiently. We’ll cover everything from electronic submission options to paper claim procedures, providing you with the knowledge you need to confidently manage your United Healthcare claim submission.
Understanding the Basics of United Healthcare Claims
Before diving into the specifics of submission, it’s important to grasp the fundamentals of United Healthcare claim submission. A claim is essentially a formal request for payment for medical services rendered. These services can range from doctor’s visits and hospital stays to laboratory tests and prescription medications. United Healthcare, as a major health insurance provider, processes a vast number of claims daily, making adherence to their specific guidelines paramount.
Each claim must include detailed information about the patient, the provider, the services provided, and the associated costs. Accuracy is key; any errors or omissions can lead to delays or denials. Understanding your policy benefits and coverage is also essential to determine what services are covered and what portion of the costs you’re responsible for.
Methods for United Healthcare Claim Submission
United Healthcare offers several methods for submitting claims, catering to different needs and preferences. The most common options include electronic submission and paper claim submission.
Electronic Claim Submission
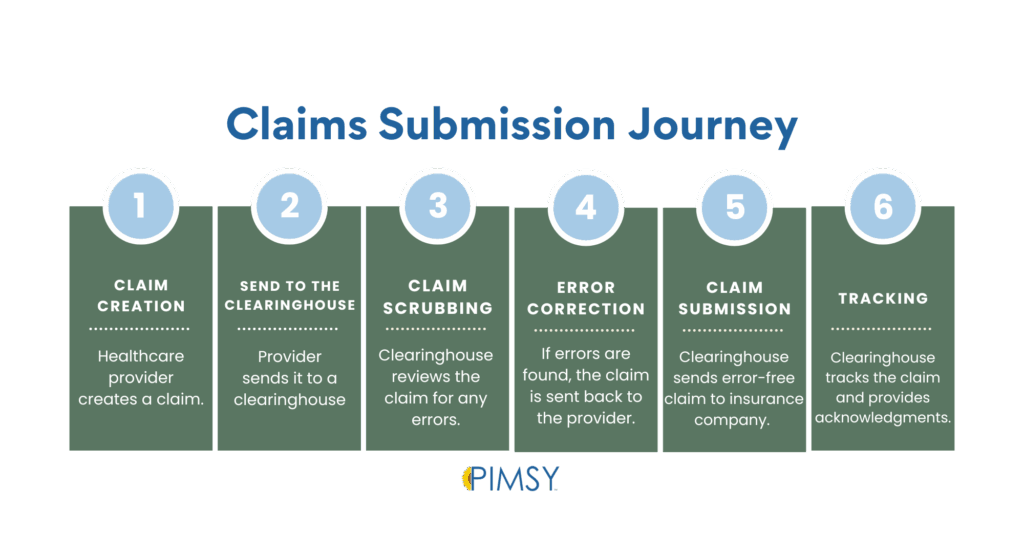
Electronic claim submission is generally the preferred method due to its speed, efficiency, and reduced risk of errors. It involves submitting claims electronically through a clearinghouse or directly to United Healthcare’s system. Many healthcare providers utilize practice management software that integrates with these systems, streamlining the United Healthcare claim submission process.
Benefits of Electronic Submission:
- Faster processing times
- Reduced paperwork
- Lower error rates
- Improved tracking and reporting
- Real-time claim status updates
To submit claims electronically, providers typically need to enroll with United Healthcare’s electronic data interchange (EDI) program and obtain the necessary trading partner IDs. Patients, however, generally rely on their providers to submit claims electronically on their behalf.
Paper Claim Submission
While electronic submission is encouraged, paper claim submission remains an option, particularly for patients who need to submit claims themselves or for providers who haven’t yet transitioned to electronic systems. Submitting a paper claim involves completing a standardized claim form (such as the CMS-1500 form) and mailing it to the designated United Healthcare claims processing address.
Important Considerations for Paper Claims:
- Ensure all information is accurate and legible
- Use the correct claim form (CMS-1500 for professional services, UB-04 for institutional services)
- Include all necessary supporting documentation (e.g., itemized bills, referral forms)
- Make a copy of the claim for your records
- Mail the claim to the correct address (verify the address on the United Healthcare website or member card)
Paper claim submission generally takes longer to process than electronic submission, and there’s a higher risk of errors or lost claims. Therefore, it’s crucial to double-check all information and retain copies of all submitted documents.
Step-by-Step Guide to United Healthcare Claim Submission
Whether you’re submitting claims electronically or via paper, the following steps provide a general framework for the United Healthcare claim submission process:
- Verify Patient Eligibility and Coverage: Before providing services, verify the patient’s eligibility and coverage with United Healthcare. This helps ensure that the services are covered under their plan and that you’re submitting the claim to the correct payer.
- Gather Necessary Documentation: Collect all relevant documentation, including the patient’s insurance card, medical records, itemized bills, referral forms (if required), and any other supporting information.
- Complete the Claim Form: Fill out the claim form (either electronically or on paper) accurately and completely. Ensure that all required fields are populated and that the information matches the supporting documentation.
- Submit the Claim: Submit the claim electronically through your clearinghouse or practice management software, or mail the paper claim to the designated United Healthcare claims processing address.
- Track the Claim: Monitor the status of your claim to ensure it’s being processed correctly. You can typically track claims online through the United Healthcare provider portal or by contacting their customer service department.
- Follow Up on Denied or Rejected Claims: If your claim is denied or rejected, review the reason for the denial and take appropriate action. This may involve correcting errors, providing additional documentation, or appealing the decision.
Common Reasons for Claim Denials and How to Avoid Them
Claim denials can be frustrating and time-consuming. Understanding the common reasons for denials can help you avoid them in the first place. Here are some of the most frequent causes of United Healthcare claim submission rejections:
- Incorrect Patient Information: Ensure the patient’s name, date of birth, and insurance ID number are accurate and match the information on their insurance card.
- Missing or Incomplete Information: Fill out all required fields on the claim form and include all necessary supporting documentation.
- Coding Errors: Use the correct CPT and ICD codes to accurately describe the services provided.
- Lack of Medical Necessity: Ensure that the services provided are medically necessary and supported by the patient’s medical records.
- Duplicate Claims: Avoid submitting duplicate claims for the same services.
- Non-Covered Services: Verify that the services provided are covered under the patient’s insurance plan.
- Prior Authorization Requirements: Obtain prior authorization for services that require it before providing them.
- Timely Filing Deadlines: Submit claims within the timely filing deadlines specified by United Healthcare.
By paying close attention to these potential pitfalls, you can significantly reduce the likelihood of claim denials and ensure smoother processing.
Tips for Successful United Healthcare Claim Submission
To maximize your chances of successful United Healthcare claim submission, consider the following tips:
- Stay Updated on United Healthcare Policies and Procedures: United Healthcare’s policies and procedures can change over time. Stay informed about the latest updates by regularly visiting their website or subscribing to their provider newsletters.
- Utilize Electronic Claim Submission: Opt for electronic claim submission whenever possible to expedite processing and reduce errors.
- Verify Patient Eligibility and Coverage: Always verify patient eligibility and coverage before providing services.
- Double-Check All Information: Carefully review all information on the claim form and supporting documentation to ensure accuracy and completeness.
- Keep Detailed Records: Maintain detailed records of all claims submitted, including copies of the claim forms and supporting documentation.
- Track Claim Status: Monitor the status of your claims regularly and follow up on any outstanding issues.
- Seek Assistance When Needed: Don’t hesitate to contact United Healthcare’s provider services department for assistance with claim submission or any other questions you may have.
Appealing a Denied United Healthcare Claim
If your United Healthcare claim submission is denied, you have the right to appeal the decision. The appeals process typically involves submitting a written request for reconsideration, along with any additional documentation that supports your claim. United Healthcare will review your appeal and issue a final determination. If you disagree with their decision, you may have the option to pursue further levels of appeal, such as an external review by an independent organization. The specific procedures for appealing a denied claim are outlined in your insurance policy documents.
The Future of Healthcare Claim Submissions
The healthcare industry is constantly evolving, and claim submissions are no exception. There’s a growing trend towards automation, artificial intelligence, and blockchain technology to streamline the claim submission process, reduce administrative costs, and improve accuracy. These advancements promise to make United Healthcare claim submission, and claim submissions in general, more efficient and transparent for both providers and patients. [See also: Understanding Healthcare Claim Adjudication] [See also: Common Medical Billing Errors to Avoid]
Conclusion
Mastering the United Healthcare claim submission process requires a thorough understanding of the guidelines, procedures, and common pitfalls. By following the steps outlined in this guide, staying informed about policy updates, and utilizing available resources, you can navigate the complexities of claim submission with confidence and ensure timely and accurate reimbursement for medical services. The key is meticulous attention to detail, proactive communication, and a commitment to staying up-to-date on the latest industry best practices. Successfully navigating United Healthcare claim submission benefits both healthcare providers and patients alike, ensuring that medical services are properly compensated and healthcare access remains seamless.
